INVITRO FERTILIZATION
Description
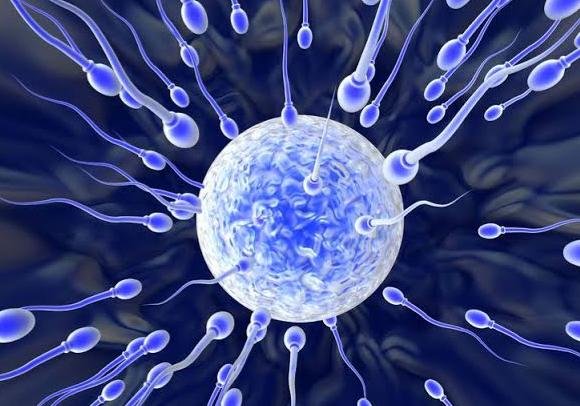
This is one of the main procedures in Assisted Reproductive Technologies(ART) where the fertilization of oocyte is done outside the female body. This procedure can be done by either a client’s own oocyte and sperm or by donated oocytes and sperm.
Why Choose IVF?
Opting for an IVF procedure increases chances of getting pregnant than using normal cycle and Interuterine insemination.
What to expect during IVF
You will be received by our team of well trained professionals that will educate and guide you through each step. IVF involves stimulation of the ovaries to produce one or multiple follicles containing eggs. Secondly, these eggs are retrieved, and fertilized with conventional IVF or Intra-cytoplasmic sperm injection (ICSI) using a prepared sperm sample to create embryos. A viable embryo is then transferred back to the uterus.

IVF may be an option in the following conditions:
Fallopian tube damage or blockage. Fallopian tube damage or blockage makes it difficult for an egg to be fertilized or for an embryo to travel to the uterus for implantation. Without a healthy fallopian tube, fertilization and implantation are affected which are very crucial steps in conception. The reason for this happening include; scar tissues, infections or pelvic adhesions.
The symptoms of blocked fallopian tubes. Most often the fallopian tube blockage is asymptomatic. Many women only realise it when they have difficulties getting pregnant.
In some cases blocked fallopian tubes can lead to mild, regular pain on the side of the abdomen. This occurs when fluid fills and enlarges a blocked fallopian tube. Conditions that can lead to a blocked fallopian tube can casue their own symptoms. Eg. Endometriosis often causes very painful and heavy periods and pelvic pain which can increase fallopian tube blockage.
Ovulation disorders. If ovulation is infrequent or absent, fewer eggs are available for fertilization.
Endometriosis. Endometriosis occurs when tissue similar to the lining of the uterus implants and grows outside of the uterus — often affecting the function of the ovaries, uterus and fallopian tubes.
Uterine fibroids. Fibroids are benign tumors in the uterus. They are common in women in their 30s and 40s. Fibroids can interfere with implantation of the fertilized egg.
Previous tubal sterilization or removal. Tubal ligation is a type of sterilization in which the fallopian tubes are cut or blocked to permanently prevent pregnancy. If you wish to conceive after tubal ligation, IVF may be an alternative to tubal ligation reversal surgery.
Impaired sperm production or function. Below-average sperm concentration, weak movement of sperm (poor mobility), or abnormalities in sperm size and shape can make it difficult for sperm to fertilize an egg. If semen abnormalities are found, a visit to an infertility specialist might be needed to see if there are correctable problems or underlying health concerns.
Unexplained infertility. Unexplained infertility means no cause of infertility has been found despite evaluation for common causes.
A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, you may be candidates for preimplantation genetic testing — a procedure that involves IVF. After the eggs are harvested and fertilized, they're screened for certain genetic problems, although not all genetic problems can be found. Embryos that don't contain identified problems can be transferred to the uterus.
Fertility preservation for cancer or other health conditions. If you're about to start cancer treatment — such as radiation or chemotherapy — that could harm your fertility, IVF for fertility preservation may be an option. Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use.
Women who don't have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry(surrogate).
You will be received by our team of well trained professionals that will educate and guide you through each step. IVF involves stimulation of the ovaries to produce one or multiple follicles containing eggs. Secondly, these eggs are retrieved, and fertilized with conventional IVF or Intra-cytoplasmic sperm injection (ICSI) using a prepared sperm sample to create embryos. A viable embryo is then transferred back to the uterus.

Fallopian tube damage or blockage. Fallopian tube damage or blockage makes it difficult for an egg to be fertilized or for an embryo to travel to the uterus for implantation. Without a healthy fallopian tube, fertilization and implantation are affected which are very crucial steps in conception. The reason for this happening include; scar tissues, infections or pelvic adhesions.
The symptoms of blocked fallopian tubes. Most often the fallopian tube blockage is asymptomatic. Many women only realise it when they have difficulties getting pregnant. In some cases blocked fallopian tubes can lead to mild, regular pain on the side of the abdomen. This occurs when fluid fills and enlarges a blocked fallopian tube. Conditions that can lead to a blocked fallopian tube can casue their own symptoms. Eg. Endometriosis often causes very painful and heavy periods and pelvic pain which can increase fallopian tube blockage.
Ovulation disorders. If ovulation is infrequent or absent, fewer eggs are available for fertilization.
Endometriosis. Endometriosis occurs when tissue similar to the lining of the uterus implants and grows outside of the uterus — often affecting the function of the ovaries, uterus and fallopian tubes.
Uterine fibroids. Fibroids are benign tumors in the uterus. They are common in women in their 30s and 40s. Fibroids can interfere with implantation of the fertilized egg.
Previous tubal sterilization or removal. Tubal ligation is a type of sterilization in which the fallopian tubes are cut or blocked to permanently prevent pregnancy. If you wish to conceive after tubal ligation, IVF may be an alternative to tubal ligation reversal surgery.
Impaired sperm production or function. Below-average sperm concentration, weak movement of sperm (poor mobility), or abnormalities in sperm size and shape can make it difficult for sperm to fertilize an egg. If semen abnormalities are found, a visit to an infertility specialist might be needed to see if there are correctable problems or underlying health concerns.
Unexplained infertility. Unexplained infertility means no cause of infertility has been found despite evaluation for common causes.
A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, you may be candidates for preimplantation genetic testing — a procedure that involves IVF. After the eggs are harvested and fertilized, they're screened for certain genetic problems, although not all genetic problems can be found. Embryos that don't contain identified problems can be transferred to the uterus.
Fertility preservation for cancer or other health conditions. If you're about to start cancer treatment — such as radiation or chemotherapy — that could harm your fertility, IVF for fertility preservation may be an option. Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use.
Women who don't have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry(surrogate).